The COVID-19 pandemic has heightened the importance of health care—and underscored its unpredictable and potentially financially devastating costs, even for middle-class households. Half of Californians delayed getting health care due to cost in the last 12 months, according to the California Health Care Foundation. For the uninsured, online fundraising to cover health care costs has become all too common. In recent years, California has taken a number of steps to improve access to affordable health care. Most notably, expanded eligibility for public health insurance through the Affordable Care Act (ACA) has significantly reduced financial barriers to necessary care. In the wake of Governor Newsom’s proposal to expand health care access to all Californians, we look at some longer-term effects of the 2014 Medi-Cal expansion in the state, with a focus on financial barriers to care.
The ACA expanded Medicaid (known as Medi-Cal in California) to most low-income adults in participating states. Numerous studies of the Medi-Cal expansion have found that it has reduced out-of-pocket health care costs, financial worries, and even debt collections and bankruptcies. But the program is also lowering financial barriers to needed health care.
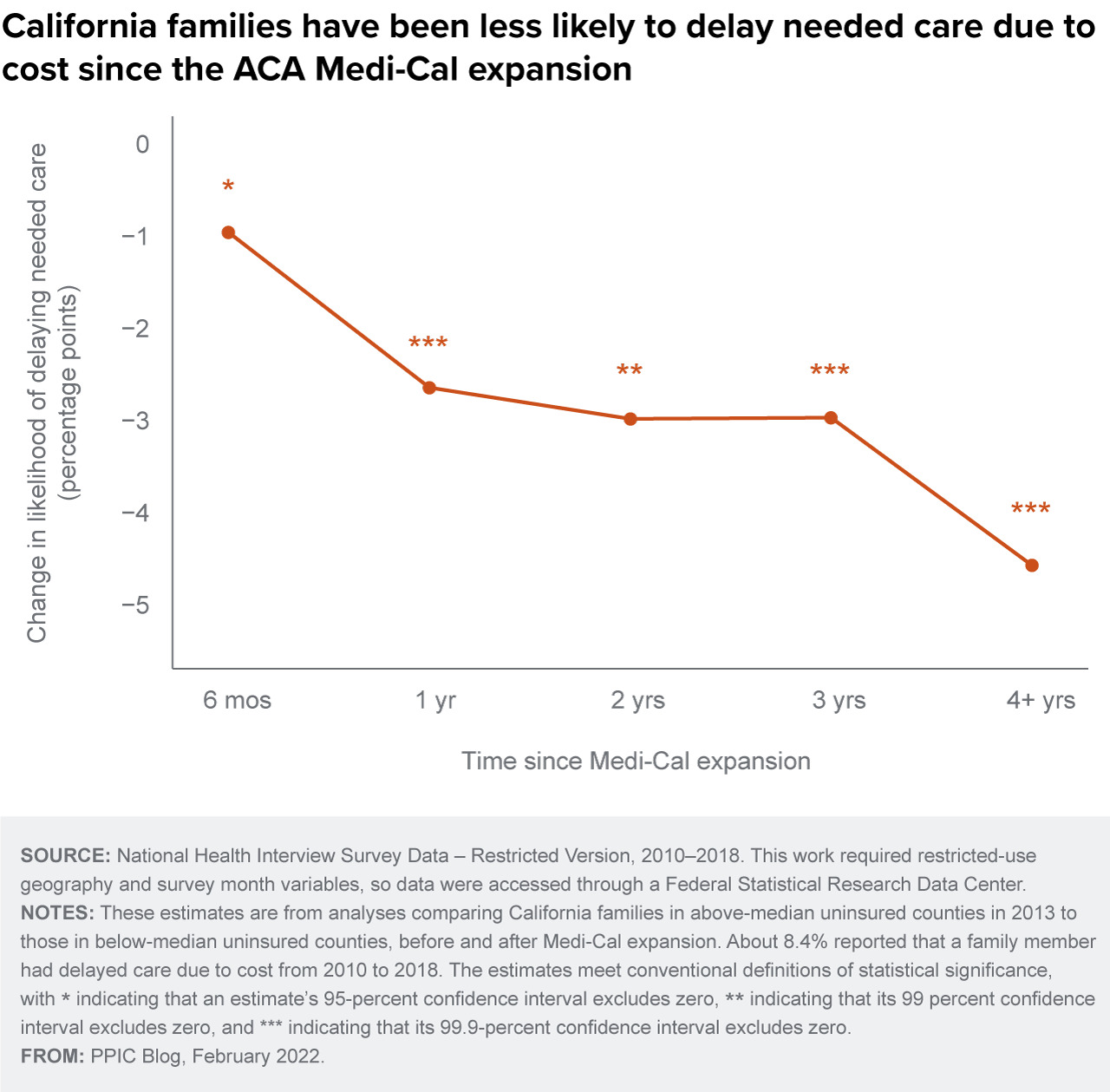
In California counties with high uninsured rates in 2013—places that stood to gain the most from Medi-Cal expansion—families have been less likely to delay needed care due to cost compared to those in other areas. Between 2014 and 2018, this translated to about a 25% reduction on average in delaying needed care. Moreover, this effect has grown over time.
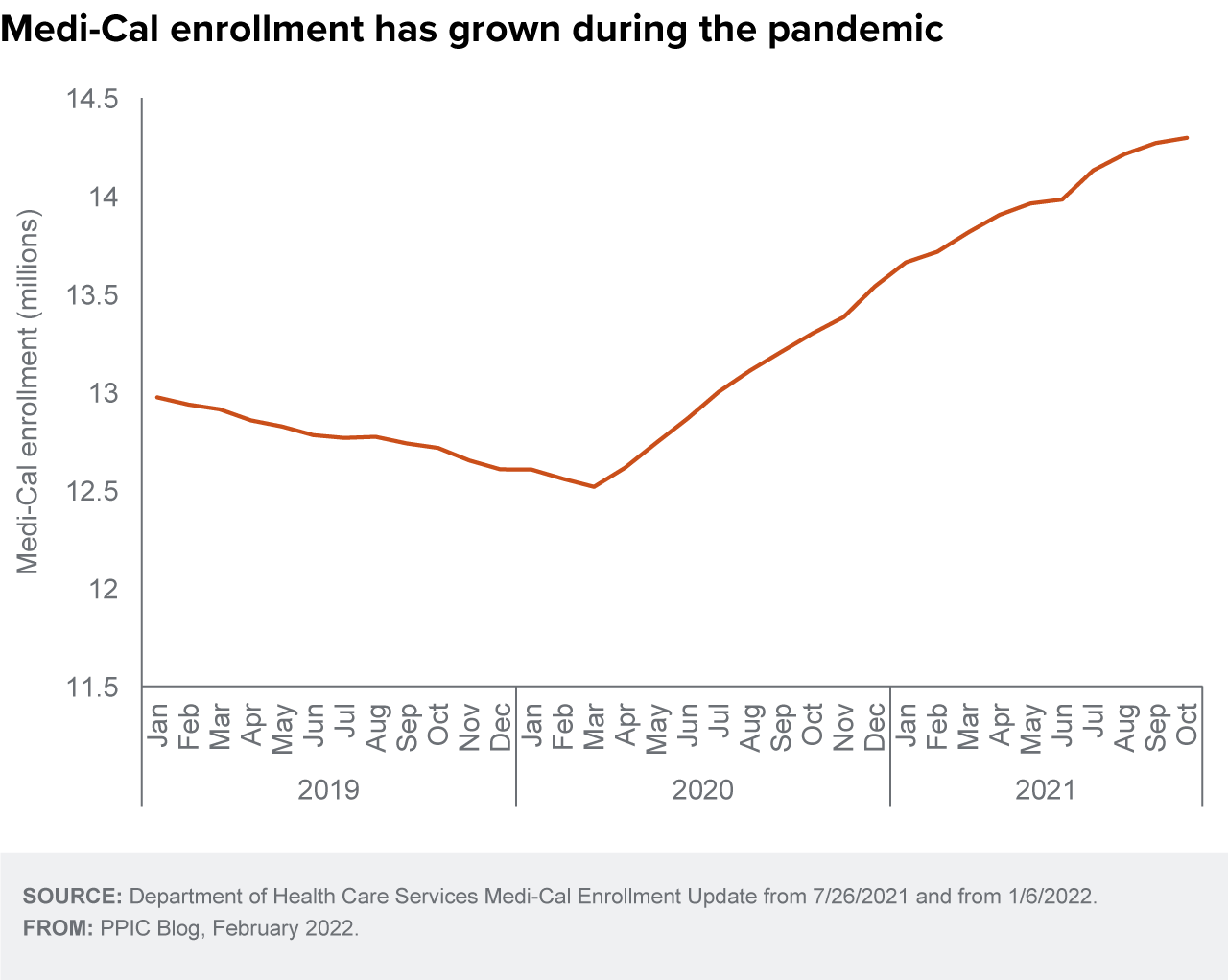
Despite Medi-Cal’s effectiveness in reducing financial stress and increasing access to health care, enrollment has been lower than expected during the pandemic: data on Medi-Cal applications during the COVID-19 period tend to show fewer new applications than in 2019. Even so, Medi-Cal enrollment has grown steadily, probably because the state paused disenrollment during the public health emergency.
The state is taking several additional steps to improve health care coverage among lower-income Californians. For example, it has expanded Medi-Cal coverage to low-income children and young adults up to age 26, regardless of immigration status, and low-income adults age 50 and over who lack satisfactory immigration status will be eligible starting May 1.
The state is also launching its newly approved, ambitious CalAIM plan to integrate Medi-Cal with social services to improve care for the most vulnerable low-income individuals. In addition, the recently established Office of Health Care Affordability aims to improve health care cost transparency—and, eventually, to reduce the cost of quality health care.
At the federal level, new protections against surprise medical billing will reduce some of the financial uncertainty associated with seeking health care. All of these initiatives have the potential to build on the ACA expansion’s success in reducing financial barriers to care.
***
Disclaimer: The findings and conclusions in this post are those of the author and do not necessarily represent the views of the Research Data Center, the National Center for Health Statistics, or the Centers for Disease Control and Prevention.
ERB approval: Data collection for the National Health Interview Survey was approved by the NCHS Research Ethics Review Board. Analysis of de-identified data from the survey is exempt from the federal regulations for the protection of human research participants. Analysis of restricted data through the NCHS Research Data Center is also approved by the NCHS ERB.




